The history of therapeutic removal is ancient, but it was not common until the beginning of the 19th century, with the invention of a guillotine.
The technique was perfected with dissection and complete removal of the tonsils and spread as a preventive action to avoid repeated infections (recurrent tonsillitis), rheumatic fever, otitis and other complications, in an era without antibiotics and with deplorable conditions of medical care, education, hygiene, housing, clothing and food.
At the beginning of the 20th century, tonsillectomy was a very popular procedure.
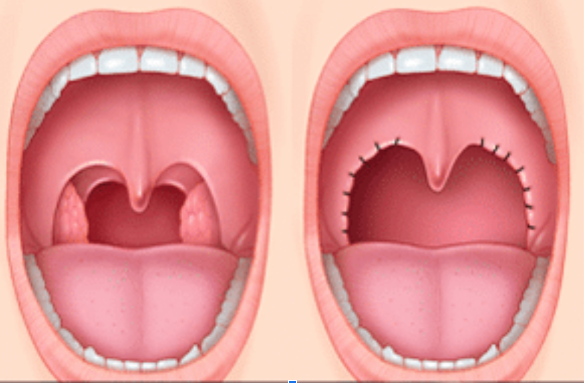
Before and After Tonsillectomy
Tonsillectomy has the potential to cause various issues, including haemorrhage, fracture of mandible condyle, glossopharyngeal paralysis and increased risk of Acute Myocardial Infarction. Cochrane Reviews display a scarcity of scientific justification for this procedure.
Evidence exposed disparities in tonsillectomy incidence between regions, suggesting arbitrary decision making and economic influence (tonsillectomy is three times more common in wealthier children than in poorer ones).
According to scientific evidence as shown carried out in a 2017 UNIFESP study 2017, Homeopathy stands out as an alternative solution for recurrent tonsillitis and hypertrophic tissues of upper airways and it can notably reduce Obstructive Sleep Apnea – OSA and Airflow Obstructions by 78%, thus avoiding the need for surgery. (Source: here)
A study published in the European Heart Journal on June 1, 2011 demonstrated that appendix and tonsil removal can lead to an increased risk of heart attack.
Surgical removal of the appendix and tonsils before the age of 20 is associated with an increased risk of premature heart attack.
According to a Swedish study in image above, those who have undergone tonsillectomy and/or appendectomy are at an increased risk of suffering from Acute Myocardial Infarction. The risk is 44% higher for tonsillectomy (hazard ratio 1.44) and 33% higher for appendectomy (hazard ratio 1.33), particularly if both operations are carried out on the same person.
“Given the strong biological and epidemiological evidence linking inflammation with coronary heart disease, it can be anticipated that surgical removal of tonsils and appendix, with its consequent effects on immunity, may also have a long-term effect on coronary heart disease,” says Imre Janszky, researcher at the Department of Public Health at the Karolisnka Institutet in Stockholm.”
This study published in the European Heart Journal examined the national health files of each Swedish citizen born between 1955 and 1970 to determine who had tonsils or appendix surgery. This data was then used to track individuals for an average of 23.5 years to check for fatal and non-fatal heart attacks (acute myocardial infarction).
The findings suggested that patients who had undergone a Tonsillectomy or Appendectomy exhibited higher prevalence of acute myocardial infarction than those who didn’t. This could be due to the fact that removal of lymphoid organs affects different components of the immune system – among them, a decrease in immunoglobulins.
The analysis underlines the impact of such procedures, which have long-term effects on immunity and modify the risk towards some autoimmune diseases.
There is already some evidence that the removal of the spleen—another secondary lymphoid organ – is associated with an accelerated atherosclerosis and increased risk of autoimmune disorders, like rheumatoid arthritis.
On 19 November 2014, Cochrane released the findings of a study affirming that Tonsillectomies carried out to combat recurrent infections and airway obstruction have little to no scientific backing.
Cochrane reviews make it clear that tonsillectomies for repeat infections lack scientific evidence.
“The impact of surgery, as shown in the included studies, is modest. Many participants in the non-surgical group improve spontaneously. The potential “benefit” of surgery must be weighed against the risks of the procedure, as adeno-tonsillectomy is associated with a small but significant degree of morbidity in the form of primary and secondary haemorrhage and, even with good analgesia, is particularly uncomfortable for Adults” Cochrane
“Surgical removal of tonsils, with or without adenoidectomy, is a common ENT operation, but the indications for surgery are controversial. Two studies in children reported that there was “no statistically significant difference” in quality of life outcomes.” Cochrane
Cochrane released a statement on 14 October 2015, indicating that adenotonsillectomy for Obstructive SleepApnea lacks a scientific basis.
Tonsillectomy or adenotonsillectomy versus non-surgical treatment of obstructive sleep breathing in children – Published October 14, 2015 – Cochrane
“It is not possible to present data on the benefits of adenotonsillectomy in children with Obstructive Sleep Breathing aged under five years, despite being a population in which this procedure is frequently performed for this purpose.” Cochrane
“For non-syndromic children classified as having Obstructive Sleep Breathing on purely clinical grounds but with negative polysomnography results, the evidence on the effects of adenotonsillectomy is of low quality and is not conclusive.” Cochrane
“Polysomnography reviews of almost half of the children managed non-surgically had normalised by seven months, indicating that clinicians and parents should carefully weigh the benefits and risks of adenotonsillectomy against watchful waiting in these children. This is a condition that can recover spontaneously over time.” Cochrane
The tonsils, or palatine tonsils, are located at the bottom of the mouth and protect the entrance to the respiratory system and digestive system, as they are part of a ring of lymphoid tissue, which facilitates the rapid response of lymphocytes to germs.
Surgical removal of the tonsils is called tonsillectomy or tonsillectomy. Adenoidectomy is the removal of the adenoids.
As mentioned before, in the beginning of the 20th century, tonsillectomy was a very popular procedure. With the increase and variability in the incidence of tonsillectomies, in 1938 the Epidemiology Section of the Royal Society of Medicine decided to study the geographical variations, the study was conducted by James Glover, a British physician:
Tonsillectomies in England and Wales showed variations of up to 17 times, suggesting arbitrary and unscientific decision-making.
The data on tonsillectomies in England and Wales showed variations of up to 17 times (annual rates of 0.3% compared with rates of 5.1%), suggesting arbitrary and unscientific decision-making.
When sharp changes in tonsillectomy rates were found, they associated the fact with changes in school physicians, For example, between 1929 and 1936, Dr Garrow reduced tonsillectomies in his area by a tenth, from 186 (2.9% of children) to 13 (o.2%), without a concomitant increase in any disease (adenitis, otitis, tonsillitis) or in school absenteeism.
Tonsillectomy was more common in upper-class children (three times as common as in the poor). There were no changes attributable to other variables analysed (climate, rurality, agglomerations, dental health, unemployment, illness, among others). Very similar adjacent geographical districts were shown to have very different rates.
Each year about 85 children under the age of 15 died as a direct and immediate consequence of bleeding in surgery. In the five years studied (1931-1935), 434 children died in these circumstances.
Data on tonsillectomies in England and Wales showed variations of up to 17-fold (annual rates of 0.3% compared with rates of 5.1%), suggesting a take on Tonsillectomies was suggested to ‘unrelated’ children, because doctors’ own children often had their tonsils preserved.
A USA study, the “fixed percentage” study, demonstrated a possible underutilization of tonsillectomies.
In 1934, the American Child Health Association launched a research project that began with 1000 randomly picked children. A first doctor determined that 40% should be operated on, and was supported by the similar suggestion from a second doctor. This was further reinforced by the third doctor’s agreement of 40%.
To the amazement of many, 65 children were not recommended to undergo tonsillectomies. This study altered the outlook of its advocates, who questioned the criteria for determining surgery.
Article published by Dr John Wennberg in the Lancet in October 2014 – “Understanding regional variation in the use of surgery”.
Dr John Wennberg, a renowned physician from the late 20th Century, studied Dr Glover’s work in the Lancet in 2014 to gain insight into why medical practice with regard to tonsillectomy was so varied.
“It is not surprising that regional variation in surgery – and its implication that many patients are getting procedures they don’t want or need.“
Dr. Juan Gérvas, Spanish physician and researcher, wrote in his 2016 book entitled “Safe and Sound”:
“In the 21st century, tonsillectomy is as alive and irrational as ever, even though several Cochrane Reviews have indicated its lack of efficacy in recurrent tonsillitis and airway obstruction. – Dr Juan Gérvas
“In Spain there is the 2006 data from the Atlas of variations in Medical Practice, led by Dr Enrique Bernal. It shows that its use was popular as adenoidectomy was the most common operation in children, followed by tonsillectomy. Like all interventions of dubious efficacy and arbitrary indication, tonsillectomy has a huge variability in Spain, of up to 13 times when comparing health areas, with rates between 3 and 39 per 10,000 children under 15 years old. In Brazil, there are data from 2014, a year in which 40,000 tonsillectomies were performed (more than half in the southeast region of the country, the richest).” Dr Juan Gérvas
According to Dr Juan Gérvas, Rheumatic Fever, which is also one of the doctors’ justifications for performing tonsillectomy, has almost disappeared from developed countries because it is a disease of poverty that is combated with improvements in hygiene, housing, clothing and nutrition.
Rheumatic Fever is an autoimmune disease caused by an abnormal reaction of the immune system against group A beta-hemolytic streptococci that infect the tonsils, skin and other parts.
“Rheumatic Fever is now a rarity and Airway Obstruction, apparently an epidemic. Tonsillectomy returns with force and with the brilliance of technology. We have overcome the “infectious theory” that justified it, to establish a “mechanical theory” that promotes it. We are going from “the child is snoring like a blessed” to “this child snores, we must operate”. The sleep of children and adolescents has been medicalised, and a variation of normality is applied, in a cruel and unnecessary way, as a technology of modernity. In the 21st century, it will be difficult for children to keep their tonsils.” Dr. Juan Gérvas.
In addition to the irrationality, there are serious risks associated with tonsillectomy. It has a mortality rate of 1 in 15,000, while morbidity is far more common; nausea and vomiting affects an estimated 90 percent of children and adolescents who undergo the procedure, but fever, haemorrhage, airway blockage, uvular swelling and mandibular condyle fracture are also factors. Further potential issues include glossopharyngeal paralysis, dehydration and pneumonia.
Homeopathy and Tonsillitis
In July 2017, the ENT department of UNIFESP/EPM (Federal University of Sao Paulo), published a clinical, double-blind, randomised Study in children with recurrent tonsillitis (Source: here):
In this scientific publication, which sought to evaluate the efficacy and safety of homeopathic treatment in children with recurrent tonsillitis who had surgical indication, the result was statistically significant (p=0.015), concluding that homeopathic treatment was effective in children with recurrent tonsillitis when compared to placebo, excluding 78% of the children from surgical indication. https://www.bvshomeopatia.org.br/revista/RevistaHomeopatiaAPHano2017VOL80Supl1-2.pdf
The homeopathic medicine did not cause adverse events in the children. (study link here)
Tonsils: lymphoid organ, defence function of the organism
It has been demonstrated that tonsils are lymphoid organs that form part of the body’s defence system. Positioned at the entrance to the oropharynx, they act as a barrier against any unwanted microorganisms.
The child’s repeated tonsillitis indicates that the tonsil is doing its job of protecting the body very well. The issue lies in the weakened immunity of the body, resulting in an increased need for the tonsil to act as a shield.
As demonstrated, a tonsillectomy will not improve your child’s immunity. In fact, this intervention can weaken the organism further by destroying one of its main defences – the tonsil – and simply shifting the non-vital problem to other organs like the pharynx, sinuses or even heart, raising the risk of an Acute Myocardial Infarction (as shown by Dr. Imre Janszky).
In other words, Tonsillectomy may mean the end of tonsil infections, but it does not guarantee better health in its entirety. In fact, the overall health of the organism may be reflected negatively.
Dr. Pedro Ozi (Sao Paulo state- Brazil),professor and homoeopathic physician, posits that all diseases can be classified into two categories: organised and non-organised.
Dr Ozi argues that infections stimulate organised responses, regulated against foreign antigens through PAMP, provide protective immunity, antigen elimination, with efficient and exonerative reactions with return to homeostasis.
As for other diseases, health conditions, including allergies, autoimmune illness, cancer and mental health concerns can lead to imbalanced, repetitive responses and the individual is unable to achieve a return to equilibrium without help. Consequently, chronic diseases are difficult to prevent.
Therefore, performing a tonsillectomy may predispose the organism to displace its illness from the organised polarity (infections – acute diseases which have a beginning, middle and end) to the disorganised polarity (allergies, autoimmune diseases, chronic diseases in general), which may cause harm and damage to the organism.
Homeopathy is a person-centered, individual/centered form of medicine that offers ethical solutions. It works by making the organism function towards recovery and a balance in its equilibrium.
It has been protecting patients for over 200 years from potential harm caused by unnecessary medical treatments.
Homeopathy has proven to be an effective treatment method for recurrent tonsillitis as well as hypertrophy of upper airway tissues, and it can even treat Obstructive Sleep Apnea Syndrome (OSAS) and Airways Flow Obstructions.
“We need to beware of the siren song of prevention, for all that glitters is not gold.”– Dr Juan Gérvas
Protect your child against unnecessary medical interventions that lack necessity and effectiveness, and may be uncalled-for.
As Dr. Juan Gérvas would say, “these interventions may have doubtful effectiveness and arbitrary origins.”
It is best practice to consult your physician of trust and, if need be, seek a second and third opinion from another knowledgeable healthcare practitioner or physician.
Gather as much valid information as you can before having to resort to any interventional practices that may prove detrimental for your child.
If you found this blog post useful, consider signing up for my newsletter. You’ll be up to date on homeopathy, natural health issues, and tips to maintain the good health of your loved ones throughout the year. Register below!
